Introduction: Treatment for chronic lymphocytic leukemia (CLL) has changed with the approval of novel agents, which have different toxicity profiles. The aim of the current analysis was to determine how incremental changes in efficacy and toxicity profile impact treatment selection among patients with CLL and oncologists.
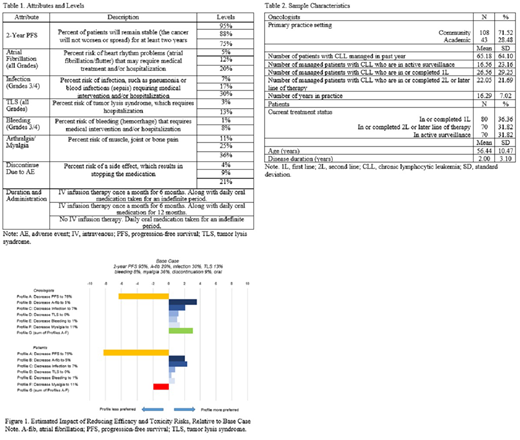
Methods: In this US-based study, oncologists and CLL patients completed an online survey that included a discrete choice experiment (DCE) to quantify preferences for first line (1L) treatment with novel agents. Self-reported data on oncologist and patient characteristics were also collected. In the DCE, respondents selected between hypothetical treatment profiles consisting of 8 attributes with varying levels. The attributes were selected based on the findings of qualitative interviews assessing treatment priorities among oncologists and patients. The attribute levels were abstracted from clinical trials and published literature (Table 1). Hierarchical Bayesian regression models were used to estimate preference weights for each attribute level.
The preference weights were used to generate a base case hypothetical treatment profile, against which other hypothetical profiles varying in adverse event (AE) risk and 2-year progression-free survival (PFS) were evaluated to understand which attributes and levels drive treatment selection. The overall mean summed preference weight for the collective set of alternative profiles was then compared with the base case, with higher positive values indicating the more preferred profile.
Results: Oncologists (N=151) reported a mean of 16.3±7.0 years in practice (Table 2). Most practiced in a community setting (72%) and in a major metropolitan/urban area (64%). Among patients (N=220), median age was 56.0 years, with a mean disease duration of 2.0±3.1 years at time of study (Table 2). Most patients were in or had completed at least 1L therapy (68%).
Figure 1 illustrates the impact of changing various attribute levels on the overall preference of an alternative profile, relative to a base case profile. Decreasing 2-year PFS from 95% to 75% (Profile A) and reducing the risks of atrial fibrillation (A-fib) from 20% to 5% (Profile B) and infection from 30% to 7% (Profile C) had the greatest influence on treatment preferences for oncologists when holding all other attribute levels constant. Oncologists preferred the profile with reduced 2-year PFS and reduced risk of AEs (Profile G) to the base case profile, corresponding to a 45% difference in preference share. Similarly, for patients, reducing 2-year PFS from 95% to 75% (Profile A) and reducing the risks of infection from 30% to 7% (Profile C) and A-fib from 20% to 5% (Profile B) were most influential in treatment choice when all other attribute levels were held constant (Figure 1). However, patients preferred the base case profile with higher PFS and higher risk of AEs to Profile G, corresponding to a 38% difference in preference share.
Conclusions: For oncologists and patients, decreasing 2-year PFS and reducing the risks of either A-fib or infection had the most influence on 1L treatment preference, relative to the base case in which 2-year PFS was the highest and the AE risks were set to the worst levels reported in literature for novel therapies. The pattern and direction of treatment preferences were generally consistent among oncologists and patients, relative to the base case, across all alternative profiles when individually examined. However, for patients, the positive impact of reducing the risk of AEs was outweighed by the negative impact of reducing PFS. Consequently, all other things being equal, patients preferred a 1L profile with higher PFS even if it came with higher AE risks. In contrast, oncologists were willing to accept a treatment with less efficacy in exchange for the most favorable safety profile. This difference may be due to a patient's lack of understanding of the potential severity of AEs or a physician's lack of awareness of the patient's treatment priorities. This is an area for future research and highlights the importance of oncologists explicitly communicating the known efficacy benefits and AE risks associated with each treatment option because these factors may influence patients' treatment choice in a way that differs from their own.
Ryan:AstraZeneca: Current Employment, Current equity holder in private company. Le:AstraZeneca: Current Employment, Current equity holder in private company. Wahlstrom:AstraZeneca: Current Employment, Current equity holder in private company. Beusterien:Kantar: Other: Employee of Kantar, which received funding from AstraZeneca to conduct this study. Will:Kantar: Other: Employee of Kantar, which received funding from AstraZeneca to conduct this study. Maculaitis:Kantar: Other: Employee of Kantar, which received funding from AstraZeneca to conduct this study. Leblanc:UpToDate: Patents & Royalties: Royalties; Agios, AbbVie, and Bristol Myers Squibb/Celgene: Speakers Bureau; AstraZeneca: Research Funding; AbbVie, Agios, Amgen, AstraZeneca, CareVive, BMS/Celgene, Daiichi-Sankyo, Flatiron, Helsinn, Heron, Otsuka, Medtronic, Pfizer, Seattle Genetics, Welvie: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; American Cancer Society, BMS, Duke University, NINR/NIH, Jazz Pharmaceuticals, Seattle Genetics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal